Two Bordetella species of bacteria regularly cause the disease known as whooping cough in humans, Bordetella pertussis and Bordetella parapertussis. Of the two, B. pertussis causes much more severe disease, with a rate of about 1 fatality per 125 cases in infants aged less than six months. As such, there has been widespread vaccination against pertussis starting in the 1940s. However, the early ‘whole cell’ pertussis vaccine (wP) was eventually replaced by the ‘acellular’ pertussis vaccine (aP), which contains proteins from B. pertussis. The aP component is typically given with diphtheria and tetanus toxoids, such as in the DTaP shot.
Those of you who follow the online exploits of various anti-vaccine groups have probably come across the factoid that a study in mice showed receipt of the acellular pertussis vaccine increases susceptibility to infection with Bordetella parapertussis to forty times compared to the unvaccinated.
For example, here’s The Refusers’ take on it:
“Vaccinators’ maniacal insistence on multiple boosters of pertussis vaccine may be the culprit behind the so-called increase in whooping cough. According to this 2010 study ‘vaccination led to a 40-fold enhancement of B. parapertussis colonization.’ In other words, the vaccine stimulates the growth of a bacterial strain that is not included in the shot. The scientific term for this phenomena [sic.] is vaccine failure.”
And here the president of the Australian (anti-)Vaccination Network states
“…it has been found that mice who are vaccinated against pertussis (whooping cough) are more likely to contract parapertussis – 40 times more likely – and parapertussis causes symptoms that are clinically indistinguishable from whooping cough. Interesting, eh?”
So ’40x’ seems to be a recurring theme, however, whether it’s increasing susceptibility to or stimulating the growth of a whooping cough-causing bacterium depends of which anti-vax source you go to. What did the study actually find?
Well, let’s look at the study, Acellular pertussis vaccination facilitates Bordetella parapertussis infection in a rodent model of bordetellosis, full text freely available on PubMed Central.
In order to study how aP vaccination influenced the course of pertussis/parapertussis infection the researchers took two equal groups of mice and immunised half with a commercial aP vaccine, and the other half with saline and an adjuvant (the placebo group). About a quarter of the mice in each group were infected with B. pertussis, another quarter with B. parapertussis, a further quarter with both bacteria, and the remaining quarter were sham-infected with saline. Then, at various time points following infection 4-5 mice from each group were euthanized, their lungs removed and the amount of each of the bacteria tested for.
The results of this experiment are summarised in this figure, and I’ll go through the four panels one by one, explaining what they represent and what it means.
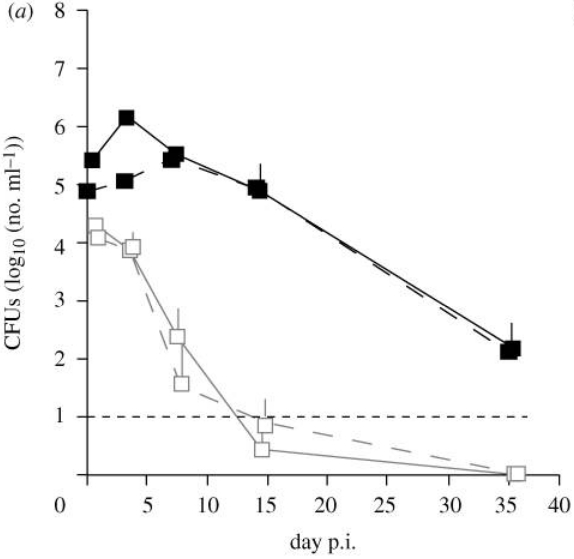
Amount of pertussis bacteria in the lungs of mice either immunised (open squares) or unimmunised (closed squares) prior to infection. Horizontal dashed line represents the limit of detection.
We’ll start with (a). As you can see, the horizontal axis is time, in days post-infection, while the vertical axis is ‘CFUs’ or colony-forming units, a measure of the amount of viable pertussis bacteria present. The filled (black) squares represent mice that received sham vaccination. As you can see, in these unimmunised mice the number of bacteria increases as the infection progresses, then as the immune response catches up, the number of bacteria falls. Now compare this to the open squares, representing aP-immunised mice. Despite all mice being infected with similar amounts of B. pertussis bacteria, you’ll notice that on day 0 there is already a ~10-fold difference in bacterial load. This means that by the time the researchers had infected all the mice (there was about 200), got that experiment cleared away, and got around to sacrificing their first lot of mice (maybe a few hours all up) the numbers of pertussis bacteria were already on the decline. This trend continues until the infection is cleared. In the unimmunised mice however, the number of pertussis bacteria increases for a few days, before the immune response catches up and brings the infection under control.
So what does this tell us? Well the fact that the immune response was protecting mice right from the time they were infected suggests that the aP vaccine reduces susceptibility to infection with B. pertussis – which has certainly been the experience with human trials. This is no surprise and is consistent with the currently available research: aP vaccination reduces susceptibility to pertussis infection and aids in the clearance of the bacterium from the respiratory tract.
What about panel (b)?
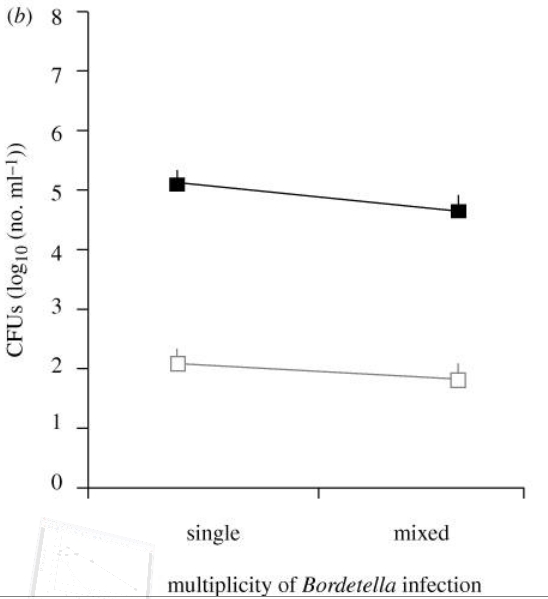
Average amounts of pertussis bacteria present in the lungs of immunised (open squares) and sham-immunised (closed squares) mice for the day 3 to 35 time points. ‘Single’ – mice that were only infected with B. pertussis; ‘Mixed’ – mice that were also infected with B. parapertussis.
The panel shows the average counts of B. pertussis bacteria from day 3-35 post infection. The two sides represent average B. pertussis counts in mice infected only with B. pertussis (left) and infected with both species (right) (This was included as the researchers wanted to test whether the two species interfered with one another in a mixed infection). As you can see, regardless of the presence of parapertussis, there is ~700 times less pertussis bacteria in those that were given the aP vaccination.
Okay, so panels (a) and (b) show aP vaccination primes the mouse immune system to be immediately ready to combat pertussis infection. So what? Why did I include them if they don’t cover the 40x figure? Well, for two reasons:
One: To familiarise readers with the format of the figure. It’s not all that approachable to those that haven’t studied some bacteriology, so before going to the parapertussis-specific data I want people to be comfortable with it, and understand what susceptibility should look like; and
Two: That data shows just how effective the aP vaccine was in combating pertussis infection, and I want everyone to enjoy just how supportive of aP immunisation this study is, and just how thoroughly it demonstrates the intellectual dishonesty of those who cite this paper, while simultaneously claiming that there’s no evidence that aP vaccination does anything to prevent/combat pertussis infection.
So now let’s look at panel (c). This is in the same format as panel (a), except the triangles indicate levels of B. parapertussis infection (that’s the one not included in the vaccine). Again, open shapes represent aP-immunised mice, closed shapes sham-immunised.
Remember, this time we’re looking at B. parapertussis:
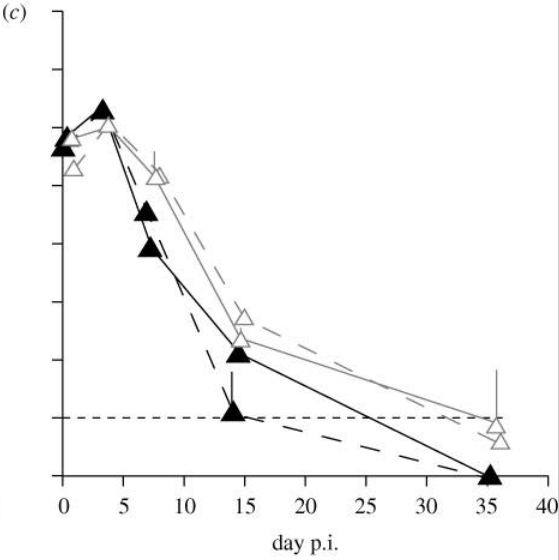
Amount of parapertussis bacteria in the lungs of mice either immunised (open triangles) or unimmunised (closed triangles) against pertussis prior to infection. Horizontal dashed line represents the limit of detection.
So what do we notice? Well in both the immunised and un-immunised the bacterial load increases, peaks at day 3, then decreases. You’ll notice that at the first two time points there is not much difference in the bacterial load of the immunised and unimmunised cohorts, but beyond then the clearance of B. parapertussis occurs more quickly in the unimmunised. It would appear that some aspect of the immune response, attributable to the aP vaccine, is interfering with the clearance of the bacterium. As a result, from days 7-35 the amount of parapertussis bacteria in the lungs of aP immunised mice is greater than in those of the unimmunised. As you can see in panel (d), from days 3-35 this difference averages at a factor of about 40x:
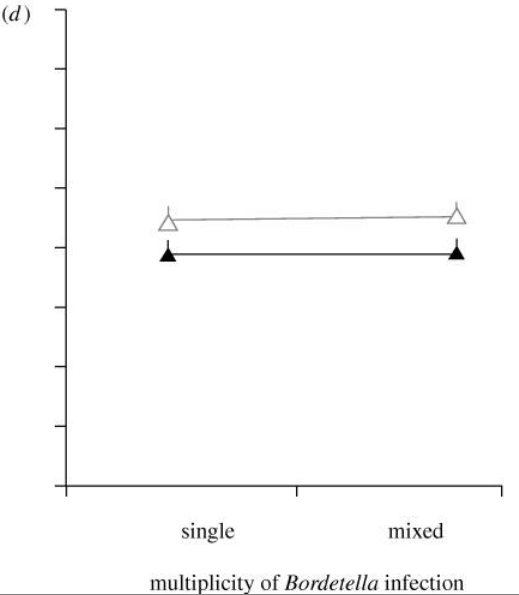
Average amounts of parapertussis bacteria present in the lungs of aP immunised (open triangles) and sham-immunised (closed triangles) mice for the day 3 to 35 time points.
So we’ve finally found the ‘40x’ figure. But is this really a measure of increased susceptibility? Well look again at panel (a), comparing pertussis infections in mice that have or have not been immunised against pertussis. Those mice that are more susceptible (the unimmunised; closed squares) show a drastically increased frequency of pertussis in their lungs compared to the immunised, which is evident from day 0. Look back to panel (c), and see that the bacterial load in parapertussis infection is indistinguishable between vaccine and sham groups for the first three days (in fact on day 3 it’s marginally lower in the aP immunised). In other words, the capacity to fend of parapertussis was uninfluenced by aP immunisation for at least 3 days following infection. So, did this study find “…that mice who are vaccinated against pertussis (whooping cough) are more likely to contract parapertussis – 40 times more likely…”? No, it did not.
That said, the time taken to clear the parapertussis infection is longer in the aP immunised. Even if susceptibility to infection if not increased, clearly something is not right. So what about The Refusers’ take, “According to this 2010 study ‘vaccination led to a 40-fold enhancement of B. parapertussis colonization.’ In other words, the vaccine stimulates the growth of a bacterial strain that is not included in the shot.”?
…not quite. Again, look at panel (c). By the time the effect is apparent, bacterial load is decreasing, regardless of vaccination status, and the only difference if the rate of the decrease. Rather than “stimulating the growth” of B. parapertussis, the effect of the vaccine is to somehow interfere with the clearance seen in the sham-immunised group. If The Refusers had looked through the article themselves and not just based their commentary on a cherry-picked quote from the press release then perhaps they wouldn’t have described bacteria whose levels are decreasing as having stimulated growth. But then again, if they based their opinions on the actual data from these studies, I guess they wouldn’t be anti-vaxxers.
So what is happening? Surely you’d expect that antibodies against B. pertussis should offer some cross protection against the related B. parapertussis?
Well, as it turns out they don’t, thanks to part of the parapertussis outer membrane called the O antigen. It seems some time in its evolutionary history, B. parapertussis resigned itself to being the less-common Bordetella species, and to try and avoid the widespread anti-Bordetella immunity in the human population induced by its more-prominent cousin, it developed an O antigen that fights antibodies. Mouse studies have shown that when the O antigen is missing, antibodies induced by both aP and wP vaccination bind parapertussis more efficiently, but when the antigen is present the binding of these antibodies is largely blocked. Luckily (perhaps ironically) the O antigen itself can be targeted by antibodies, which is important for inducing anti-parapertussis immunity.
Okay, so the O antigen research explains how aP-induced immunity is rendered ineffective against parapertussis, but the study in question didn’t just show no effect on parapertussis from aP immunisation, it showed an impairment of the clearance of the bacterium. The researchers asked why, and found less neutrophils were recruited to the lungs of parapertussis-infected mice when they’d received aP immunisation.
Neutrophils are the most common white blood cell in the blood, and are the first to flood to the scene of an infection, where they effectively destroy microbial invaders. Recruitment of these cells to the respiratory tract and targeting to Bordetella cells by antibodies is critical for the optimal clearance of both pertussis and parapertussis.
So why were less neutrophils recruited to the lungs of parapertussis infected mice that previously received aP vaccination? Well the researchers looked into the type of immune responses, and found that unvaccinated mice exposed to either bacterium developed more of an inflammatory response, which is more effective in recruiting neutrophils, while the immune memory induced by the aP immunisation favoured a less-inflammatory response.
While this bias in the kind of immune response induced is not a problem in pertussis infection (just look at panel (a) again – it is clearly protective) it seems that this has actively impaired the response to B. parapertussis.
While the researchers did not divine the exact mechanism behind the impaired clearance of parapertussis, these clues they found do allow for well-informed conjecture. It would appear that the less-inflammatory response the vaccine pushes the specific immune response towards impaired neutrophil recruitment. While that isn’t a problem in subsequent pertussis infection, parapertussis uses its O antigen to further impair immune responses, buying the bacterium a little more time.
The authors note that this study was done in mice, and should not be simply extrapolated to humans, though I answer the question of whether this effect is seen in humans here. In short, our biggest prospective trials of aP vaccines come up negative when it comes to the question of aP immunisation in any way enhancing parapertussis infection.
I’d like to finish this post with one last observation. Last month, PLOS Medicine published a study examining how ‘spin’ on a research article can be translated to inaccurate reporting, by comparing the abstracts, press-releases and finally media reports on those articles to see where the exaggerations were introduced. For a plain-language summary, I’d suggest reading Dr Novella’s coverage of the paper on Neurologica. Not unsurprisingly, it was found that scientists’ overselling of their own findings in the abstracts of their articles was highly correlated with spin in the subsequent reports in the media.
When it comes down to it, the ultimate message I take from the PLOS Medicine study is that scientists need to frame their findings and conjecture carefully when writing abstracts. Over-hyping results or their relevance might be eye-catching and possibly increase your chances of getting into a better journal, but is ultimately a dishonest act and should be avoided.
I felt the entire body of the parapertussis study was a good assessment of the results and their implications. However, this was the abstract:
Despite over 50 years of population-wide vaccination, whooping cough incidence is on the rise. Although Bordetella pertussis is considered the main causative agent of whooping cough in humans, Bordetella parapertussis infections are not uncommon. The widely used acellular whooping cough vaccines (aP) are comprised solely of B. pertussis antigens that hold little or no efficacy against B. parapertussis. Here, we ask how aP vaccination affects competitive interactions between Bordetella species within co-infected rodent hosts and thus the aP-driven strength and direction of in-host selection. We show that aP vaccination helped clear B. pertussis but resulted in an approximately 40-fold increase in B. parapertussis lung colony-forming units (CFUs). Such vaccine-mediated facilitation of B. parapertussis did not arise as a result of competitive release; B. parapertussis CFUs were higher in aP-relative to sham-vaccinated hosts regardless of whether infections were single or mixed. Further, we show that aP vaccination impedes host immunity against B. parapertussis—measured as reduced lung inflammatory and neutrophil responses. Thus, we conclude that aP vaccination interferes with the optimal clearance of B. parapertussis and enhances the performance of this pathogen. Our data raise the possibility that widespread aP vaccination can create hosts more susceptible to B. parapertussis infection.
I was flabbergastered on re-reading the abstract, specifically the last line; “Our data raise the possibility that widespread aP vaccination can create hosts more susceptible to B. parapertussis infection.”
The only point in the article such a concept is raised is in the introduction, where they discuss hypothetical mechanisms by which parapertussis could have an advantage over pertussis in an aP-immunised population. The data certainly do not raise this possibility, which would explain why the authors do not mention it when interpreting their data. The inclusion of that sentence at the end of the abstract is a perfect example of over-hyping results to sell your study.
Even worse is the press release, written by one of the study’s authors:
“…vaccination led to a 40-fold enhancement of B. parapertussis colonization in the lungs of mice…”
“…these data suggest that the vaccine may be contributing to the observed rise in whooping cough incidence over the last decade by promoting B. parapertussis infection”
I do not have a problem with that first sentence; an enhancement of colonisation or an impairment of clearance, either way it’s a matter of semantics, though I do feel ‘impaired clearance’ more accurately describes the observed effect. As for the second sentence, the only place in the study that possibility is implied is the abstract; the data show nothing of the sort.
Looking at the two sentences together it’s easy to see how the misconceptions were bred. It’s just a shame that second sentence is simply untrue.
Scientists should know better.

Pingback: The whooping cough vaccine doesn’t increase your odd of getting any kind of whooping cough! | The LymphoSite
Great explanation, thanks Tom, very clear. I’d love to take this study a step further and see if there are clinical or perceptual differences, rather than just statistical differences. What I mean is if the immune response has been shifted to reduce inflammation, would that make a difference in how people infected with parapertussis feel? And if it takes longer to clear the bacteria do people feel sick for longer? Are they infectious for longer?
Of course you’ve already pointed out that the effect does not appear to happen in humans so it’s a moot point. But us scientist types (or non-scientist anti-vaxxers) need to keep in mind the differences between statistical and clinical significance when working with medicine.
Pingback: Anti-vaccine chiropractors 8 | reasonablehank
Pingback: Anti-vaccine chiropractors 36 | reasonablehank