Before reading this post be aware that as of April 2014 we now know that Australian strains of B. pertussis have largely lost expression of the protein whose variation is a key feature of this piece. An explanation of that study can be found here.
Summary
Whooping cough is a potentially deadly infectious disease. While vaccination against it has managed to significantly reduce the incidence of the disease, it still remains a global presence.
Recent coverage in the mainstream media and from anti-vaccine proponents has suggested that the whooping cough bacterium has evolved around the current acellular vaccine. Such reports occurred following publication of a paper attributing over 80% of Australian cases to a new strain apparently not well covered by the vaccine.
This review analyses these claims. Careful examination of the current literature indicates that while the bacterium’s genome does appear to have changed in response to pressure from the vaccine, none of these changes appear to give it any significant advantage over the immunity the vaccine induces. Thus, reports that the current vaccine is ineffective are misleading and inaccurate. Each of the factors that could potentially influence vaccine-induced immunity are discussed.
You may remember about a fortnight ago in the news there were references to a new study which looked at an emerging strain of whooping cough and raised some questions about the current vaccination campaign. Intrigued, that very day I downloaded and read the paper in question, as well as the previous paper from the same group. What followed was a fortnight in which my spare time was taken up by reading as many journal articles as possible about whooping cough and the vaccine.
Then, just a few days ago, Meryl Dorey, president of the Australian Vaccination Network, wrote a blog post attacking the current whooping cough vaccination program, in which she cited this new, fascinating research (funnily enough, with an explanation that suggests she hasn’t actually read it). It strikes me that a reply to this blog post would be an ideal format for a piece discussing the history, efficacy and new insights into the whooping cough vaccine, so here goes.
It seems that the president of the anti-vaccine lobby group The Australian Vaccination Network is at it again, vilifying people who have suffered from vaccine-preventable diseases and misrepresenting the state of medical research.
In a new ironically named blog post, ‘the fear that transcends logic’, Ms Dorey attacks a mother living “in the heart of the avn’s kingdom… surrounded by anti vac people” whose family contracted both whooping cough and chicken pox, despite being fully vaccinated. The open letter explains the terrible circumstances the family has gone through dealing with whooping cough, in an attempt to give others some insight into coping with the disease.
However, neither the contents of this letter, nor how Ms Dorey treats the writer are the focus of this post. This post will deal with the incorrect information Dorey has provided about the whooping cough vaccine.
Right off the bat Dorey sets the scene:
“Our biggest problem is that both the government and the medical community have painted parents who don’t vaccinate or who vaccinate selectively as ‘the enemy’. They are intentionally vilifying the unvaccinated without any evidence that we are the problem. In fact, they are consciously choosing to ignore the medical research proving that the pertussis or whooping cough vaccine is almost completely ineffective against the strain of the disease circulating in Australia today (84% of all whooping cough cases are being caused by bacteria that is not contained in our current vaccine and it is possible that the vaccine itself was responsible for this change in the strain of bacteria which is now responsible for whooping cough).”
Is this the case? Has the bacterium responsible for causing whooping cough mutated so much that it’s not affected by vaccine-induced immunity, and all because of the vaccine?
First, some background. In the 1950s a whooping cough vaccine was introduced, and saw a massive drop in cases all around the world. However, the vaccine had a high rate of side-effects such as seizures, dizziness and fainting, which led to decreased uptake of the vaccine, and a subsequent resurgence of disease. This vaccine contained whole, killed cells of Bordetella pertussis, the whooping cough bacterium, and it seems that the fact that the entire organism was in there was behind the severity of the reactions. In order to reduce the rate of adverse events, a new vaccine was introduced. The new ‘acellular’ vaccine, which replaced the whole-cell vaccine in Australia in 2000, contains just a few proteins produced by B. pertussis, one being the pertussis toxin (chemically inactivated, of course), and the other two (which I’ll call Prn and FHA for now) being adhesion molecules, which basically help the bacterium cling to the host’s respiratory tract.
Here it’s worth noting that there exist other formulations of acellular pertussis vaccines, which contain two more adhesion molecules, as well as formulation with just one or two components. But, as the three-component vaccine is the most commonly used form in Australia it’s what I’ll be referring to when I use the term ‘acellular pertussis’ or aP vaccine.
So what is the efficacy of the acellular pertussis vaccine? Well, in an attempt to answer that question, the Cochrane Collaboration put together a review of all the existing literature, entitled “Acellular vaccines for preventing whooping cough in children”. The review, updated in March of 2012, considered only double-blind randomised placebo controlled trials in which participants were actively followed up and cases of pertussis were laboratory verified – in other words, only the very best evidence. In the end, they included six studies of aP vaccine efficacy, which investigated vaccines with a variation of 1-5 acellular pertussis components. They found:
“This updated review included six efficacy trials with a total of 46,283 participants… The efficacy of multi-component (≥ three) acellular vaccines varied from 84% to 85% in preventing typical whooping cough (characterised by 21 or more consecutive days of paroxysmal cough with confirmation of B. pertussis infection by culture, appropriate serology or contact with a household member who has culture-confirmed pertussis) and from 71% to 78% in preventing mild pertussis disease (characterised by seven or more consecutive days of cough with confirmation of B. pertussis infection by culture or appropriate serology). One- and two-component acellular vaccines were less effective.”
So the vaccine is quite effective, and quite logically, the fewer pertussis proteins included, the less effective the shot in preventing the disease.
One of the concerns about using a vaccine with only a few components is that it should be easier for the microbe to evolve around. That is, when an entire pertussis cell is in the vaccine, then potentially every molecule in the bacterium could hypothetically be the target of an immune response; when just three pertussis molecules are in the vaccine, protection is less broad. If the bacterium mutates its three vaccine-targeted molecules enough then eventually they’ll be so different that aP vaccine-induced immunity won’t recognise them, whereas with the whole cell vaccine there’s far more vaccine targets to mutate, making that version of the vaccine so much harder to evade.
Another issue with the current vaccine is the waning of vaccine induced immunity. A recent literature review put the duration of vaccine-induced immunity at 4-12 years (although it looks like the figure can be optimised by careful timing of booster shots), as opposed to 4-20 years for naturally acquired infection. This is something that will need to be sorted out with the next generation of pertussis vaccines as people are notoriously bad at getting their boosters, to the point where only an estimated 11.3% of the adult population of Australia is up to date on their whooping cough shots.
So, has B. pertussis managed to mutate its pertussis toxin, Prn and FHA proteins to the point where the immunity induced by the vaccine versions of them is seriously impacted, making our current estimates of aP vaccine efficacy wrong?
Well, no.
In fact, the bacterium has only mutated two of the three proteins – the FHA most commonly used by B. pertussis in Australia is the same as the kind in the vaccine. However, FHA is one of the less important vaccine targets involved in protection from pertussis, and so the fact that they still match isn’t all that big a deal. Let’s get onto the mismatches.
Firstly, pertussis toxin. Acellular pertussis vaccines include the active subunit of pertussis toxin, referred to as PtxA. Genetic variants in PtxA are then numbered, eg: PtxA1, PtxA4 etc. Studies have shown that pertussis toxin is the most important pertussis protein to include in the vaccine for inducing a protective immune response, with some experts even suggesting that a one-component pertussis toxin vaccine is all that would be necessary to induce effective immunity.
The current Australian aP vaccines contain PtxA2, while all samples of B. pertussis isolated recently from Australia express PtxA1 – definitely a mismatch. But how does that impact the current statistics? Well, from what I can tell, not at all.
“What?” I hear you ask, “How on earth can you think that efficacy data from a vaccine containing pertussis toxin variant 2 can be generalised to a country in which the endemic pertussis strains carry toxin variant 1?”
“Well,” (I would respond) “because those efficacy trials were *done* in populations where the endemic pertussis strains carry toxin variant 1!”
That’s right. There is a mismatch between the vaccine type pertussis toxin and the type our wild strains carry, but that doesn’t change the efficacy data because that same mismatch existed in the population it was collected from. Looking at the three studies the Cochrane Collaboration included that studied three or more component vaccines, the countries and years they took place in, there is an at or near 100% rate of PtxA1 in the wild B. pertussis population. [See Note 1]
So what about the last remaining protein in the Australian aP vaccine, pertactin, or Prn? After all, in the recent study of Australian Bordetella pertussis samples, 86% of the 194 collected were positive for a specific non-vaccine Prn variant, Prn2, whereas the vaccine contains Prn1. These two forms of the protein differ by only a few amino acids (the building blocks of proteins) in an area of the protein called ‘variable region 1’. Apart from this, the proteins are identical.
Pertactin is a cell-surface protein of B. pertussis which assists in bacterial adherence to host cells. A study in mice demonstrated that antibodies to pertactin, but not other pertussis proteins were essential for efficient opsonisation (the process where antibodies bind a bacterium or virus and mark it for destruction by white blood cells). So, surely a mismatch between vaccine and circulating variants of Prn could have an effect on vaccine efficacy?
A study using an animal model of pertussis infection published in 2001 suggest this could indeed be the case. In this paper the researchers found that the Dutch whole cell pertussis vaccine (which includes Prn1) was significantly more protective against Prn1 strains than Prn2 strains. Two years later a study looking at human serum samples (serum being the fraction of blood that contains proteins such as antibodies) tried to see if they could find Prn1-specific antibodies in serum from people who’d received booster shots, and from people who’d been infected with Prn2-carrying pertussis. Of course, they found Prn1-specific antibodies in 68-84% of children who’d received booster shots, but only in 0-6% of kids that had had a Prn2-type pertussis infection.
So there is type-specificity in the human immune response to pertactin. Does this mean that the estimate of vaccine efficacy we currently use is likely not to apply to these currently circulating Prn2-carrying strains?
Well no, because the human immune response to pertactin is almost entirely directed against parts of the protein that are the same between Prn1 and Prn2. A study published in 2008 took human serum samples and measured how well they react to different parts of the pertactin protein, and found that two of the thirty seven samples they collected showed significant reactivity to variable region 1, compared to 36 of the 37 reacting to the N-terminus of the protein, which is a region that is identical in Prn1 and Prn2. These results don’t make the previous study wrong. What the first study found was that pertactin induces type-specific antibodies. What the second study found was that yeah, it does, but those antibodies are pretty insignificant compared to the amount induced against type-indifferent parts of the protein. The authors conclude:
“Combined, these results suggest that variation in Prn will probably not constitute a problem in highly immune individuals, as we were unable to measure any antibody differences in this group. However, in individuals with low antibody [levels] and waning immunity this has to be investigated further.”
So in other words, if you’ve just got your booster, the response you’re developing doesn’t care whether any invading B. pertussis is Prn1, Prn2, or whatever Prn type, but it’s possible that these type specific antibodies might play a bigger role once vaccine-induced immunity begins to wane.
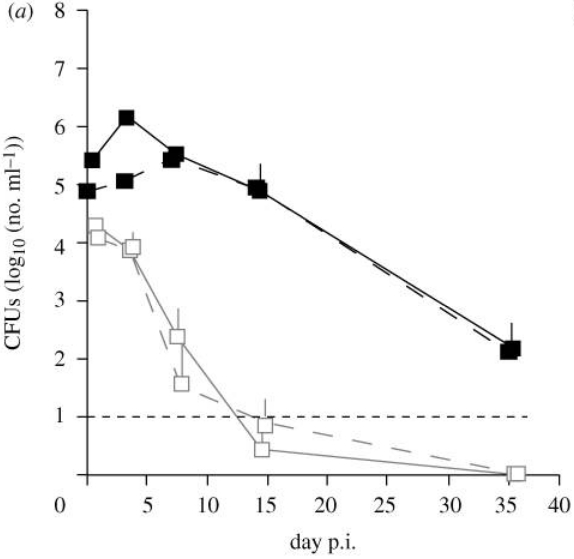
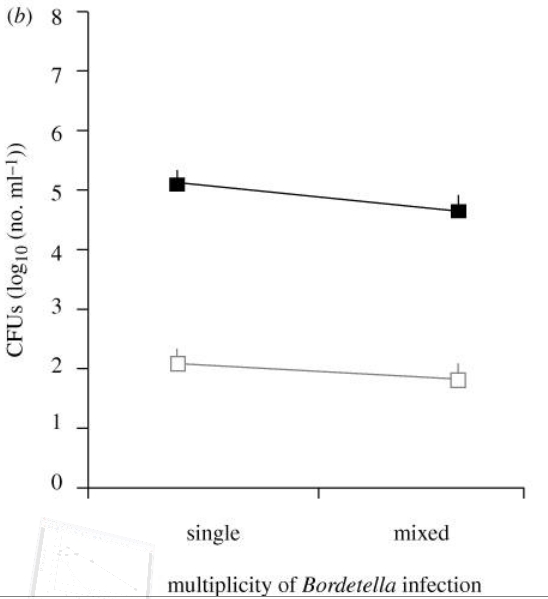
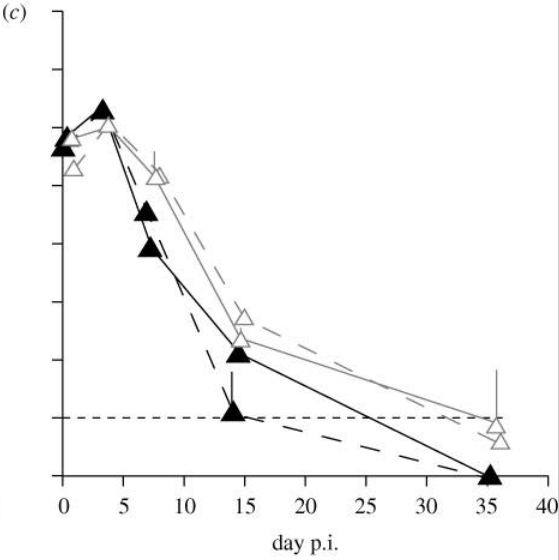
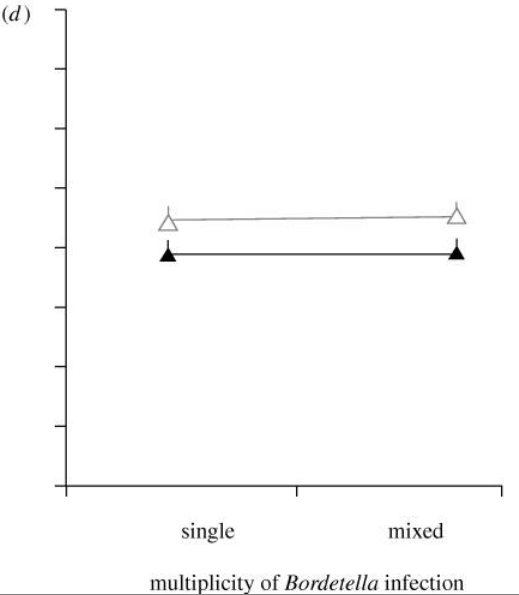
Okay, so neither of the individual variations in vaccine-targeted proteins seems to suggest that any considerable change to our current estimation of vaccine efficacy is needed, but what about the combination of the two mutations? Well, a paper published in May 2010 wanted to establish how these new, non-vaccine variations in PtxA and Prn could be impacting vaccine efficacy. They immunised mice with a current PtxA2 and Prn1-containing aP vaccine, and then infecting them with four different varieties of B. pertussis. All four were derived from the same strain as the vaccine, except three were genetically modified so that:
- In one PtxA2 was replaced with PtxA1
- In another, Prn1 was replaced with Prn2
- And in the third, both PtxA2 and Prn1 were replaced with PtxA1 and Prn2, respectively.
As you might expect, the authors found a statistically significant difference between the number of pertussis bacteria in the lungs of the immunised mice challenged with the vaccine strain, and those challenged with the double mismatch mutants. However, it’s worth noting that while the double mismatch challenged mice had ~10 times more pertussis bacteria in their lungs compared to those challenged with the vaccine strain, they still had 100 times fewer pertussis bacteria than the unvaccinated controls.
However, that doesn’t inform the current question of whether the varieties currently circulating in Australia might warrant a change in the current efficacy estimate, since the aP vaccine trials were done in human populations challenged with a pertussis toxin mismatch. So, in the mouse study, was there a difference between the bacterial loads of immunised mice challenged with pertussis toxin single mutants and the bacterial loads of immunised mice challenged with toxin/pertactin double mutants? Yes, there was a slightly greater bacterial load in the mice challenged with the double mutants, but the observed difference was not statistically significant.
So, what effect do the mismatches between the vaccine-strain and circulating pertussis strains have on our current estimates of vaccine efficacy? Well, the pertussis toxin mismatch has no effect, since the efficacy data was done in populations with this mismatch, while the animal and human data suggest that the pertactin mismatch gives the pertussis bacterium at best a negligible advantage, and even then most likely only manifesting in any considerable manner in the population with waning (either vaccine-induced or wild Prn1-carrying pertussis-induced) immunity.
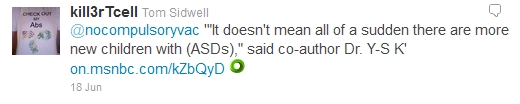
So as well as attributing her claim that the vaccine is almost useless against the emerging pertussis variants to this new paper (the paper does not say that – it is just not true), Dorey also cites the paper, saying:
“The new strain of pertussis (whooping cough) is far more dangerous than the older strain. It produces much higher levels of pertussis toxin and it is the toxin that determines how bad the symptoms will be. (Newly Emerging Clones of Bordetella pertussis Carrying prn2 and ptxP3 Alleles Implicated in Australian Pertussis Epidemic in 2008–201; The Journal of Infectious Diseases 2012;205:1220–4)”
Funnily enough, none of this over-hyped fear-mongering actually appears in the paper she’s citing as a source. But before I get into the data regarding possible enhanced virulence of this new emergent variant, I’d like to address a minor point of pertussis bacteriology Ms Dorey butchers here.
“…and it is the toxin that determines how bad the symptoms will be.”
While the pertussis toxin is one of the major virulence factors of B. pertussis, it is not the only one. In fact, it is not the only toxin the bacterium produces. In fact, the closely related species B. parapertussis is capable of producing a pertussis-like syndrome, despite the fact that it is incapable of producing pertussis toxin. What’s more, comparing genome sequences of pertussis bacteria with and without this new mutation has revealed that it is associated with mutations in at least two other virulence-associated genes, the reactivation of a gene that was previously mutated to the point where it was inactive, the inactivation of two more genes, as well as a deletion of a chunk of the genome encoding eighteen genes. Ascribing a change in virulence to just one mutation when there are this many other mutations also present in these same strains seems premature, especially since the significance of any or all of them really hasn’t been established yet.
Just keep an eye out for such over-simplifications of complex scientific issues, as Ms Dorey has done here. More often than not, they’ll turn out to be wrong.
So this claim of Dorey’s relates to this new paper I mentioned, which looked at 194 Australian pertussis samples from 2008-2010 and found that 86% of them carried the mutation ptxP3. This mutation is a change in one DNA base in the pertussis toxin promoter (the part of the genome that controls how much pertussis toxin is made). How dangerous is this mutation? Well, a 2009 paper looked at toxin production of ptxP3-carrying pertussis cells in culture, and compared the frequency of pertussis hospitalisations and deaths from two time periods where ptxP3 frequency went from 1.6% to 54.5% in the pertussis population. The researchers cultured pertussis cells with different ptxP variants for 48, 54 and 60 hours on agar plates (on a solid jelly-like growth medium in petrie dishes) and found that ptxP3 variants produced 1.62 times the amount of pertussis toxin that other strains did. It’s unclear exactly how this relates to toxin production in humans, though it seems reasonable to assume that ptxP3 strains will also express more pertussis toxin in an infection than non-ptxP3 strains. Is 1.62x ‘much higher levels’ of toxin production? Well, the term’s subjective, but in this context, I’d say it doesn’t warrant the hyperbole Meryl attributes to it, especially since we don’t even know what the rate of secretion is like in an actual infection.
So what about the hospitalisation and death data? Well, the authors calculated ‘lethality’, the number of deaths divided by the number of hospitalisations, and found that in 1981-1992 lethality was 0.00041 deaths per hospitalisations compared to 0.00299 in 1993-2004. And while those numbers may seem small, that equates to a seven-fold increase in lethality. Sounds pretty bad, right? Well, it may be. While I expect there would be an increase in the number of cases and deaths from whooping cough associated with this ptxP variation, the 95% confidence interval (basically a measure of the possible error within certain parameters, like error bars) for the lethality figure varies from 0.93-56.07 – all the way from a slight decrease in lethality, to a ridiculously over-the-top increase. What’s more, there’s more factors involved in the numbers of hospitalisations and deaths from pertussis than just which ptxP variant is most common. At this stage there just isn’t enough data to allow a confident estimation of how much more virulent ptxP3 strains are. Are they more virulent? Probably, in my opinion. Can we reasonably say they’re ‘far more dangerous’? Not just yet.
Meryl Dorey also claims the vaccine isn’t effective, and even goes on to say
“In fact, there is a great deal of evidence that not only won’t these vaccines prevent the diseases they are meant to – but that those who are vaccinated and catch the diseases may have worse symptoms than those who are unvaccinated and contract them (the exact opposite of what the medical community claims).”
Wow. Ms Dorey claims her authority comes from 20 years of researching vaccines, yet despite this, she can’t provide a single reference to support her assertions. In all of the efficacy trials the Cochrane Collaboration considered acceptable for inclusion in their aP vaccine review, in every single one, the rate of laboratory confirmed pertussis infection is lower in the vaccinated. So, from reading the best evidence available, one could easily be forgiven for thinking that acellular pertussis vaccines are effective at preventing pertussis infections, and certainly not at causing it. But, luckily for anyone who was foolish enough to base their opinion on that kind of evidence, Meryl Dorey is here to correct that impression with her collection of unsourced, uncited statements. While she may not actually provide any studies to back these claims up, if you’re lucky she’ll tell you just how numerous such studies are.
She finishes her screed against the pertussis vaccine by saying
“Healthy, unvaccinated children are no more likely to spread infectious diseases than healthy vaccinated children”
Whether they’re healthy or not isn’t the point, the point is whether they’re more susceptible to contracting pertussis or not, which the efficacy trials have been quite definitive about, but let’s read on.
“And being fully vaccinated – or even being immune (which is a totally different situation altogether) cannot prevent you from carrying and transmitting infectious diseases even if you yourself are not showing the symptoms as Dr Larry Palevsky so clearly demonstrated in his blog.”
So what does this blog post, from December 2011, say? Well, Dr Palevsky begins by discussing the outbreak of pertussis in Suffolk County, New York State. He begins by rightly stating that the actual number of cases of whooping cough is likely higher than the ~200 reported at the time. He then goes on to lament the fact that the health department is reporting the number of cases but – shock and horror – they are not also reporting the vaccination status of each case!
“Simply reporting the total number of cases of pertussis without reporting their vaccination status is also incomplete, and misleading to the public.” [bolding mine]
If Dr Palevsky honestly believes that, during the outbreak of a deadly disease, the health department should be prioritising data collection and analysis over, say, I don’t know, co-ordinating a response to the outbreak, then he should get his head out of his rear-end, or at least out of his private clinic, and go work in public health for a while.
Interestingly, he then goes on to state that an outbreak of ~200 cases really isn’t all that bad, and that it’s an over reaction to tell people to go out and get their boosters. Yes, I know this seems to contradict his first point, which says that the actual number of cases will actually be higher than the reported number, but we’ll just skip past that for now.
He then states the current pertussis vaccination rate for 19-35 month and 13-17 year old children in the area of the outbreak, and there’s a range of 75-95% vaccination uptake across the age groups and areas. So he has up-to-date pertussis immunisation rates. Does he use these figures to do a back-of-the-envelope calculation of how many susceptible kids there should hypothetically be in the area of the outbreak? No. he ignores those figures and instead cites a 1995-2001 telephone survey which attempted to quantify and analyse the numbers, counties and various details (race, reasons for exemption etc.) of completely unvaccinated 19-35 month olds in America. He takes the average rate of completely unvaccinated kids across the country from the survey, 0.3%, and applies it to the county the outbreak is in. When he discovers that this rate is so absurdly low that it can’t possibly explain the outbreak (by some unstated criterion), he decides this must mean that it’s mathematically impossible for unvaccinated children to have some big role in the spread of pertussis.
All that Dr Palevsky demonstrates with this is his own ignorance of the whooping cough vaccine. It is not just the unvaccinated that are more susceptible to catching, and therefore spreading pertussis, it is also those who have been vaccinated, but not against pertussis, as well as those who have been vaccinated against pertussis, but whose immunity has since waned, not to mention the vaccinated that are still susceptible to disease (remember, the vaccine doesn’t work 100% of the time, it has an estimated efficacy of ~71-85%). The idea that only the unvaccinated are susceptible to pertussis is a strawman, which Dr Palevsky clearly finds it easier to attack than the actual efficacy data.
He then goes on to say:
“Pertussis bacteria live in the air. They get blown around along with the other trillions of bacteria that live in the air. Because pertussis bacteria live in the air, we breathe them in along with the other trillions of bacteria swirling around. They end up inhabiting our noses, airways, and lungs. We can be harboring pertussis bacteria in our airways simply by breathing the air.”
Well, no. B. pertussis is an obligate human pathogen. That is, it has to inhabit a person to survive, replicate and grow. What is true is that an infected person can spread pertussis to another person by respiratory droplets – that is, they hitch a ride on the microscopic drops of moisture released when an infected person coughs. What is not true is the picture Dr Palevsky paints of B. pertussis as the aerial equivalent of plankton. They don’t just swirl around on the breeze, inhabiting every square meter of the air around us. It’s a finicky organism that requires some very specific conditions in order to be able to grow and survive. If you’re in a room with an infected person, then it may be a more accurate representation (in the unvaccinated there is an ~80% transfer rate of pertussis to household contacts), but pertussis bacteria are not just always swirling around us in our every day lives.
At last, he finally raises a point that might actually be valid, that is, asymptomatic carriage of pertussis. It is possible for B. pertussis to colonise someone’s respiratory tract and not cause disease. It’s even possible for a vaccinated person to be colonised by B. pertussis, and then come down with whooping cough once their immunity wanes. During the time they are carrying it they could potentially pass it on and infect other people. Because of this Dr Palevsky equates the vaccinated and unvaccinated in their potential to carry and pass on pertussis.
While it’s true that the effect of asymptomatic or mild cases in the vaccinated on transmission remains to be established, it’s not like we’re clueless. Take for example this paper, the first hit if you search PubMed for ‘pertussis outbreak asymptomatic’. The study looked at an outbreak of pertussis in a daycare, in which all four unvaccinated children contracted the pertussis, whilst of the remaining 27 vaccinated children, two contracted pertussis, one with milder symptoms than the unvaccinated cases, the other with no symptoms. Here there was one vaccinated child found to be asymptomatically harbouring pertussis. Does this mean we need to re-evaluate our estimates of vaccine efficacy, because this skews the stats? Well, no, because when pertussis is detected in an asymptomatic vaccinated individual it’s still considered to be a ‘case’. It doesn’t skew the stats, because in more recent studies where all exposed individuals are tested for the presence of the whooping cough bacterium, asymptomatic cases are identified, and so far no studies have come out saying that the rate of asymptomatic cases they’ve found is inconsistent with the current estimates of vaccine efficacy. In fact, the World Health Organisation specifically note that “chronic carriers of B. pertussis are uncommon“. In other words, there’s not currently any good evidence that a high rate of asymptomatic pertussis carriage is occurring in vaccinated kids and somehow making them as likely to pass on pertussis as the unvaccinated, and studies, such as the one above, where the exposed are tested regardless of symptoms or not, are evidence against this ludicrous argument, as is the frankly low rate of this carriage.
So, in short, all Dr Palevsky’s blog post proves is that he didn’t do any background reading into the bacteriology of Bordetella pertussis or into the vaccine against it. Dorey’s claim that “being fully vaccinated – or even being immune (which is a totally different situation altogether) cannot prevent you from carrying and transmitting infectious diseases even if you yourself are not showing the symptoms” is fallacious; the rate of asymptomatic carriage in the vaccinated is low enough that vaccinated children can’t be considered equally as likely as the unvaccinated to spread pertussis, especially since the efficacy studies demonstrate they are less likely to contract the infection than unvaccinated controls.
And Meryl Dorey finishes with a corker:
“Vaccines create antibodies – they do not create immunity. So when a vaccinated person gets a disease they are supposed to have been protected against, the vaccine has failed in its job. The community has not failed – the vaccine has. And if vaccines can’t protect individuals – they can’t protect at all.”
Let’s break it down.
“Vaccines create antibodies – they do not create immunity.”
Actually, aP vaccines have been demonstrated to induce strong both T and B cell responses against pertussis, and what do you call a lower infection rate in vaccine recipients compared to placebo recipients if not evidence of immunity?
“…when a vaccinated person gets a disease they are supposed to have been protected against, the vaccine has failed in its job. The community has not failed – the vaccine has. And if vaccines can’t protect individuals – they can’t protect at all.”
So according to Meryl Dorey, unless the aP vaccine protects 100% of recipients 100% of the time, it’s worthless. This is an astonishingly ignorant statement from her that makes me wonder: does she wear a seatbelt?
The huge disconnect between the literature I’ve read over the last fortnight and what I’ve read in Ms Dorey’s blog post was astonishing, and to be honest, I felt embarrassed reading it, when it became obvious that she hadn’t even read the one paper she cites for support. As well as attributing to it frankly hyperbolic doomsaying, the phrase of hers:
“84% of all whooping cough cases are being caused by bacteria that is not contained in our current vaccine”
…is clearly meant to relate to this paper, and is also clearly wrong. Firstly, the paper states that 100% of the pertussis samples taken are caused by bacteria not in the vaccine, right in the introduction, when it notes that PtxA1 is the only variant of the pertussis toxin active subunit found in Australian B. pertussis. If, instead, she were going by the Prn mismatch, the figure would have been 86%, not 84%. The 84% figure is actually the percentage of B. pertussis samples that had both the Prn2 and ptxP3 variants; I expect that’s the sort of nuance you would miss if you didn’t actually read the paper you were citing and got your interpretation of it from newspaper headlines.
And lastly, for the claim by Ms Dorey I am yet to address: is the vaccine responsible for the observed changes in which strains are predominant (that is, the observed shift to Prn2 and ptxP3)? Well, from my reading of the literature, the general consensus seems to be along the lines of ‘yeah, that seems to make sense’. Vaccination against B. pertussis provides strong selective pressure, as demonstrated by the severe reductions in the genetic diversity of the species when a vaccine is introduced, and both of these mutations contribute, each in a small way, to evasion of our immune responses. Firstly, as mentioned, it looks like, in a population vaccinated with Prn1, immunity to Prn2 wanes sooner, giving pertussis cells carrying this version a very slight advantage over Prn1 pertussis. The vaccine doesn’t select for Prn2, it selects against all Prn types – just a little less effectively against Prn2 cells than Prn1. Secondly, greater production of pertussis toxin (a la ptxP3) should theoretically give pertussis a little extra leeway time to set up its infection, replicate and get passed on to a new host, thanks to the suppressive effects the toxin has on our immune responses. However, this should not be advantageous in the recently immunised, as they have existing anti-toxin antibodies that can simply mop up the toxin and allow clearance of the bacteria; this would be most advantageous during the infection of someone without prior pertussis infection or immunisation, or whose immunity has waned.
So, both of these adaptations by the whooping cough bacteria sound like a win for them and a lose for us, right? Well, not so. In researching this I made some observations which I think are actually quite heartening. Firstly, in a mouse model of pertussis infection, Prn2 was found to be associated with decreased respiratory colonisation. Secondly, the closely related species B. parapertussis and B. bronchoseptica both carry the genes for making pertussis toxin, but in both species the promoter region is so mutated that they are unable to produce it. What this tells us is that there is a cost to producing pertussis toxin, a cost high enough that both of these species don’t do it any more. And yet, across the world, B. pertussis is moving toward increased pertussis toxin production.
This species has made two changes that before vaccination would be considered maladaptive, probably in order to try and evade vaccine-induced immunity, and yet the advantages it has received for these changes are, as I’ve discussed, relatively small.
The pressure that vaccination has put on this species is immense, to the point where it is making otherwise maladaptive changes in order to try and evade the vaccine.
We have Bordetella pertussis on the ropes. These recent developments on the side of the bacterium are desperate, but most importantly, they are not working.
We can send this species the way of smallpox. We can send it the way of rinderpest.
In the long run we’re going to need a vaccine with longer lasting immunity, and as I type this, research around the world into such vaccines is continuing, but for now, the acellular pertussis vaccine remains our best way of preventing B. pertussis infection. Right now, you can do your bit to help protect yourself, your family and your community from whooping cough. My last booster was in August 2005, seven years ago. Chances are I’m about to be entering the period in which my anti-Prn2 immunity begins to wane, before the anti-Prn1 immunity starts to go too. This week I will be calling up my local medical clinic and booking in an appointment for my adult booster shot. You can do the same thing too, and together we can help relegate this pathogen to the sands of time, where it belongs.
[Note 1: The three studies mentioned were conducted in Germany, Italy and Sweden. The PtxA1 prevalence data across Europe is summarised in this review, with specific figures for each country here: Germany, Italy, Sweden.]
(P.s. You may notice that in the Blog post by Meryl Dorey she also attacks the Chicken Pox/Shingles vaccine. The reasons I didn’t address that part of her blog post were twofold. The minor reason was length, as clearly this was a long post with just the pertussis-relevant sections. The major reason was that every single one of her incorrect/misleading claims about the shot were effectively answered by the ‘Varicella’ and ‘Zoster’ sections of the Australian Immunisation Handbook, and so there wasn’t really any fun background reading to do.)