This post is a discussion of the April 2014 study showing Australian pertussis bacteria to be losing expression of the vaccine target pertactin. The post describing the evidence that the pertussis vaccine does not increase susceptibility to parapertussis is here.
Finally, more information has come out about the proportion of Whooping Cough bacteria that are losing expression of a protein targeted by the current vaccine.
The background it relatively simple: from the 1950s a vaccine against whooping cough was used that contained whole, killed cells of the bacterium responsible for the disease, Bordetella pertussis. Although the biggest studies to date have failed to support the claims, contemporary fear–mongering led to an increase in rejection of the vaccine and in lawsuits filed against its manufacturers and a subsequent shortage of the shot. Part of the solution to the drop in public confidence was the development of a vaccine that only contained several key proteins of the pertussis bacterium, the acellular pertussis (‘aP’) vaccines. In Australia, the whole cell vaccine was fully phased out of routine childhood immunisations in the early 2000s, with an aP shot containing three pertussis proteins currently on the childhood schedule.
Last year, an American report noted that of 12 clinical isolates (that is, samples of the bacterium obtained from sick patients) of Bordetella pertussis they tested, 11 had lost expression of Pertactin (Prn), one of the proteins included in modern formulations of the aP shot. Given that the version of the shot subsidised for the childhood schedule only includes three pertussis proteins, one of which is Prn, there is the possibility that this loss, if widespread, may have serious implications for the effectiveness of the immunity induced by the vaccine. As I predicted in my coverage of that paper, Australian researchers have since addressed the questions of how frequent these Prn-negative strains are and how recently they’ve arisen. In this post I will try to summarise for non-biologists the April 2014 paper, Rapid Increase in Pertactin-deficient Bordetella pertussis Isolates, Australia.
The juicy bits of the paper are summarised in their Figure 2 (below) which shows how many isolates from each year did or did not have detectable Prn expression (the bars) and what percentage overall were negative (the line).
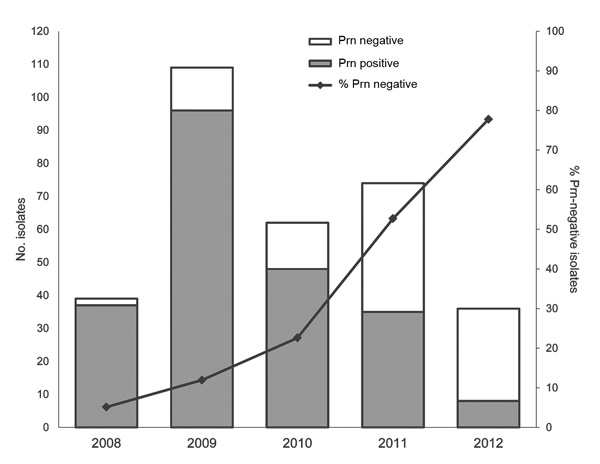 The authors report only being able to detect Prn-negative strains from 2008 onward, with a sharp rise that culminates in ~80% of isolates lacking detectable Prn protein in 2012. This suggests that there may be a selective advantage for Prn-negative strains of B. pertussis.
The authors report only being able to detect Prn-negative strains from 2008 onward, with a sharp rise that culminates in ~80% of isolates lacking detectable Prn protein in 2012. This suggests that there may be a selective advantage for Prn-negative strains of B. pertussis.
In order to determine whether this was a single chance event which gave one strain superiority, or possibly a more widespread loss of Prn protein expression in the wild B. pertussis population, the researchers decided to sequence the gene that normally encodes for Prn protein to see why it had been lost.
Interestingly, the team discovered that there were multiple reasons for the block in protein production. 80% of Prn-negative isolates had insertion sequences – pieces of mobile DNA, sort of like mini-viruses that jump through the genome – smack bang in the middle of the gene, stopping production of the protein. Two of the 96 Prn-negative isolates seemed to have complete deletion of the gene. Sixteen of them had completely normal Prn genes, indicating some other factor regulating production of the protein must have been altered. All of these mechanisms again differed from those reported by researchers outside of Australia who reported Prn-negative pertussis isolates. In short, there have been multiple roads to Prn-protein negativity taken by the pertussis bacteria, which suggests there has been a strong selective pressure on it for so many ways of losing the protein to have spontaneously arisen in the B. pertussis population.
So what does pertactin loss mean? From the vaccine effectiveness standpoint, if we assume near-complete loss of Prn expression, then our most-used vaccine now effectively only targets two pertussis proteins, PtxA (the active subunit of the pertussis toxin) and Fha (filamentous haemagglutinin – used by the bacterium to stick to things, such as our respiratory tract). As I described last time, the biggest prospective, randomised, placebo-controlled clinical trials of aP vaccines that only target these two proteins showed an effectiveness of 59-69% which equates to a 2.4-3.2 greater rate of pertussis disease in the unvaccinated controls compared to those who got the shot. While these figures are indeed suboptimal when compared to many other vaccines on the childhood schedule, it shows that targeting PtxA and Fha alone can mediate protection from pertussis.
What about the effect of Prn protein loss on the bacterium? Well, the authors point out previous work that found Prn-mutants were less able to colonise mouse respiratory tracts, but those that managed to colonise were more able to invade the cells lining the tract and persisted for longer. The authors also point out work that found Prn-deficient mutants grew faster in the lab than the Prn-expressing bacteria they were derived from, but it’s unclear whether that has any relevance to an infection scenario – the fewer other proteins the bug has to produce the more resources it can dedicate to reproducing, but the loss of a protein that helps colonisation may not be worth it in an infection.
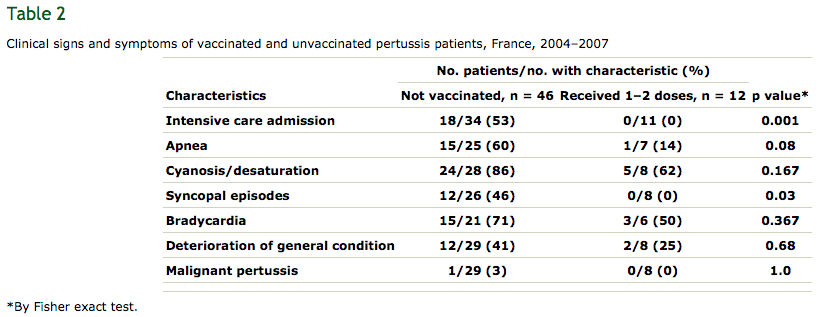
Lastly, covering the relevance of Prn loss to clinical outcomes, the authors discuss a recent French retrospective study which compared the health outcomes of infants that had infections with Prn-positive or -negative B. pertussis. Prn-negative infections were found to induce no worse clinical symptoms than Prn-expressing ones, consistent with earlier mouse work from the same group which found Prn-negative isolates to be no more lethal. The French study also found infants with Prn-negative infections spent on average four days less time in hospital than Prn-positive infections, suggesting the loss may negatively impact the bacterium’s ability to cause severe disease, though the sample size was not big enough for the difference in hospital stay times to reach statistical significance. Lastly, the French group found that, regardless of Prn expression, immunisation against pertussis was significantly associated with protection from the worst of the disease – just have a look at their Table 2, below:
 In summary, Australian Bordetella pertussis bacteria are increasingly losing expression of pertactin protein. This apparently global trend by the species, with multiple mechanisms of loss (and even by the closely related species Bordetella parapertussis), is consistent with this being a response to vaccine-induced selective pressure. However, both human and animal data indicate that Prn loss does not worsen disease, and shows that the pertussis vaccine is still the best broadly available protection from whooping cough.
In summary, Australian Bordetella pertussis bacteria are increasingly losing expression of pertactin protein. This apparently global trend by the species, with multiple mechanisms of loss (and even by the closely related species Bordetella parapertussis), is consistent with this being a response to vaccine-induced selective pressure. However, both human and animal data indicate that Prn loss does not worsen disease, and shows that the pertussis vaccine is still the best broadly available protection from whooping cough.
The long-term solution to the problem of the bacterium slowly evolving around the immunity induced by the vaccine is a new, more broadly-acting vaccine. And, as I’ve discussed before, there are several whole cell variants in various stages of testing being reported in the literature. In the short-term, people should get their adult boosters and protect themselves from pertussis disease. I got mine last year, making sure to ask for the five-component variant (Adacel in Australia), in the hope of that extra protection.
It’s quite clear now that there’s a problem, with the whooping cough bacterium gradually accruing mutations which should afford it some protection from immunity induced by the vaccine. I hope in the coming months we will see some sensible action by the Australian Technical Advisory Group on Immunisation, as I don’t want to see what the national pertussis statistics may look like in a decade if this problem is not addressed soon.

Pingback: Has Whooping Cough Evolved Around The Current Vaccine? Reflections On The (Then) Current Scientific Evidence | The LymphoSite
Pingback: ‘Vaccine resistant’ pertussis – in a way, yes. In a more accurate way, no. | The LymphoSite
Pingback: Waning pertussis immunity in England/Wales, and bad reporting in Australia | The LymphoSite
Its really great post you have shared about the protein expression, that how it helpful in the research and development.